For at least the last three decades, US healthcare providers have been struggling to improve the quality of care. But what exactly does quality of care mean? Referring to the Hippocratic oath (“first, do no harm”), we may assume that quality of care is about patients’ safety. The Agency for Healthcare Research and Quality (AHRQ) defines safety more prosaically as “freedom from accidental or preventable injuries produced by medical care.”
Medication errors are one of the most common causes of preventable injuries and side effects among hospitalized patients in the practice of modern medicine. The US Food and Drug Administration (FDA) states that there are more than 100,000 reports of hospitalizations in the US each year associated with a suspected medication error.
Such errors may result in financial and reputational damage for medical practices, increased emergency department visits, and prolonged hospital stays. Furthermore, according to Statista, 44,000 to 98,000 deaths among patients in the US hospitals annually are linked to medication errors. This death toll incurs a global cost of approximately 326 million US dollars. However, the loss of human life is the highest price. Not surprisingly, clinics are concerned with how to minimize risks. That’s the main purpose of custom healthcare software development.
Custom healthcare software helps to ensure the correct medical care. E-prescribing solutions, also known as eRx software, are now an essential part of the eHealth industry. These healthcare solutions aim to ease daily challenges for patients, physicians, and pharmacies.
For instance, patients often have difficulties confirming drug availability at pharmacies, reading instructions, confirming insurance coverage, and getting refills. For doctors and pharmacists, it’s exhausting to search through piles of medical records and recall drug information (contraindications, allergies, side effects) to advise on treatment.
Simplify medication management with an eRX system
We deliver secure eRX solutions that easily integrate with your other healthcare systems
When do medication errors usually occur?
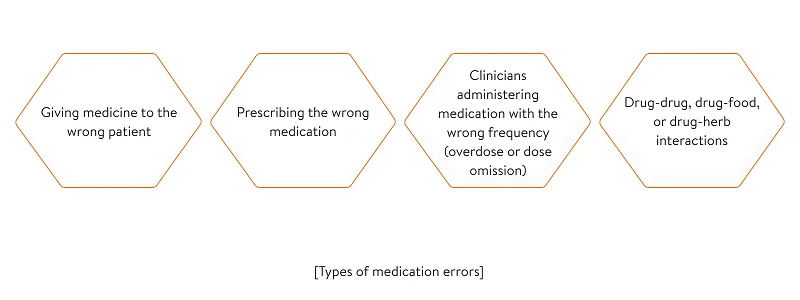
Medication errors are usually associated with:
Adverse drug events – a burning problem for clinicians
The abovementioned medication errors can lead to what’s known as an adverse drug event (ADE). An ADE can happen when medications are taken or prescribed inappropriately. ADEs are the cause of a staggering 1.3 million emergency room visits each year in the US hospitals according to the Centers for Disease Control (CDC). Moreover, the World Health Organization points out that low- and middle-income countries suffer from 134 million adverse reactions per year.
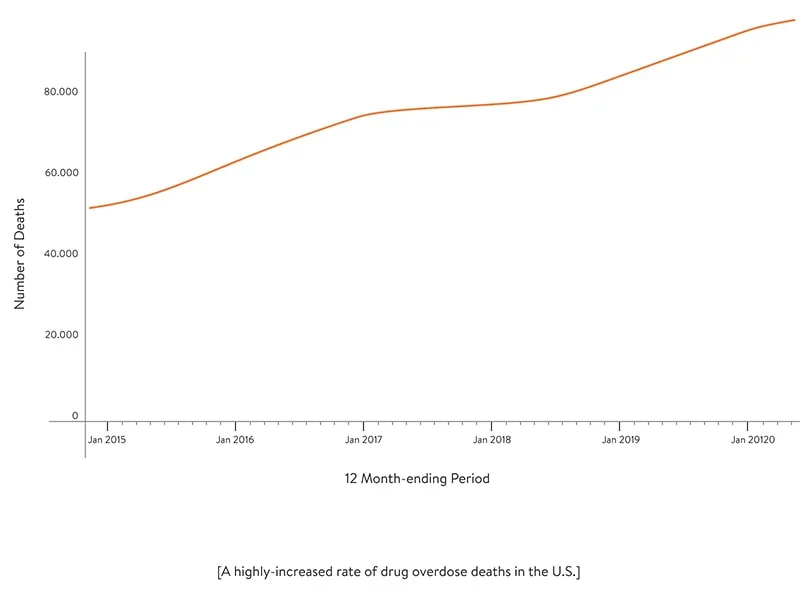
But these studies are based on pre-pandemic data from 2018–2019. No doubt self-medication during the COVID-19 pandemic has escalated the rate of adverse drug events. The global pandemic increased the use of non-confirmed drugs in large doses. This even led to a shortage of some drugs including hydroxychloroquine, azithromycin, and ibuprofen. Furthermore, the pandemic has exacerbated the opioid crisis in the US. According to CDC statistics (based on data available analysis on 7/4/2021), there was a 29.4 percent increase in synthetic opioid overdose deaths in the US compared to the previous year.
Thus, the pandemic has only heightened the importance of e-prescribing solutions.
At what stages of the medication journey do errors usually happen?
Usually, medication mistakes occur at these stages:
- Ordering\prescribing. A doctor might select the wrong drug from a drop-down menu, forget to prescribe a drug, prescribe an improper dose, prescribe a similarly named drug, or prescribe an unauthorized drug.
- Documenting\transcribing. A pharmacist may replace the prescribed drug with an alternative without the physician’s approval. This alternative can lead to unintended side effects.
- Dispensing. A pharmacist may fail to validate the prescription (by confirming the patient’s personal information). A pharmacist can also give a patient expired medication, an incorrect drug, or the wrong dosage (if age or weight weren’t clarified). Errors may also occur when a pharmacist creates the wrong label for medication. A pharmacist also might not identify drug–drug interactions.
- Administering. Errors at this stage usually happen when a pharmacist, nurse, physician, or certified medical technician gives the drug to the wrong patient or provides a patient with an extra dose.
- Monitoring. A doctor may fail to identify and document possible drug incompatibilities, allergic reactions, or side effects.
Risks at the stages of dispensing and administering medications are usually associated with issues exchanging information among healthcare professionals (physicians, pharmacy benefit managers, pharmacists). But it’s not always human factors that are to blame for medication errors.
Let’s figure out what advantages custom eRx software can provide.
Key benefits of efficient e-Prescribe application software
The good news is that handwritten prescriptions are no longer an obstacle. As of 2020, 84 percent of healthcare providers had switched to e-prescriptions. But poorly implemented healthcare software – particularly in terms of its design and interfaces – can cause harm as well. Dr. James L. Madara, the Executive Vice President and CEO of AMA, claims that most medical software and applications are not designed to ease physicians’ needs. This forces medical practitioners to seek replacements for their existing systems.
Custom eRx software was born to facilitate the traditional drug prescription process and reduce medical errors associated with illegibility, including mixing up drug names, dosages, and forms. It also should help to minimize the number of phone calls to confirm prescriptions, formularies, and refills. All this can result in a better workflow and greater productivity for pharmacy staff as well as increased patient satisfaction.
Below we give a short summary of the main benefits of a smart and effective eRx solution. This summary is based on our experience building e-Prescription software.
Learn how we enhanced an EHR system with an eRX module to enrich customer experience
Read the case studyBenefit verification
Having access to a patient’s insurance information, eRx software provides a more effective and quicker way to see formulary lists and choose medications that are covered by a patient’s drug benefit policy, allowing prescribers to choose the most clinically appropriate but still cost-effective treatment option for a patient.
Automated clinical decision support and faster medication reconciliation
It’s impossible for clinicians to keep all drug-related information in mind. Many drugs come in numerous forms and strengths; moreover, you should be careful about drug interactions, allergies, and side effects. E-prescribing lets doctors look up drugs and read prescribing instructions. It also speeds up the process of generating and filling prescriptions thanks to drop-down lists and default sig information (instructions for patients as to how much medication they should take, how they should take it, and when).
And by having access to patients’ charts and historical medical data, an eRx system can also offer clinical decision support by sending alerts on contraindications, dangerous doses, potential adverse reactions, and duplicate therapies to caregivers while providing clear instructions to clinicians on how to provide better treatment.
Increased medication adherence and fewer unfilled or lost prescriptions
Patients can forget to fill their prescriptions, lose them, or decide not to take medicine at all. As a result, around 20 percent of paper prescriptions go unfilled. eRx mobile app development provides an effective way to track unfilled prescriptions, allowing doctors to remind patients about the necessity of taking medication using in-app chat or email. This helps to increase medication adherence. Doctors can also use eRx tools to track the frequency with which patients fill prescriptions for controlled substances, making it easier to detect potential drug abuse.
Simplified prescribing of controlled substances
Thanks to integration with the Prescription Drug Monitoring Program (PDMP) database, e-prescribing tools can let prescribers check a patient’s history of controlled substance use. This database also allows for more effective tracking of Schedule II–V drugs, which can help to cut the increasing rates of opioid-related addiction, abuse, and death. All measures provided by the PDMP prevent drug-seekers from altering prescriptions or doctor shopping for controlled drugs.
There is also the DEA initiative which regulates the e-prescribing process of controlled substances under existing federal law. Below, we will discuss safety measures included in the DEA requirements.
Faster prescription refills
Physicians and clinical staff say that responding to prescription refill requests is their greatest burden. E-prescribing makes it easier for patients to get refills. It’s also easy for clinicians to process urgent refills using eRx software.
Making sure your eRx delivers real value to end users
By having access to patients’ prescription histories and checking for contraindications, age, weight, allergies, and diagnoses, eRx software can help clinicians avoid prescribing the wrong or a duplicate drug. It’s also possible to help providers define the most effective yet affordable medication options by being connected to pharmacy benefit management technology and enabling access to insurance benefit information. For these and many other reasons discussed above, progressive software vendors strive to upgrade their eRx software by integrating it with other systems.
Based on our experience, we share the structure of customized eRx systems and the role of eRx integrations below. Here’s how information is exchanged between e-prescribing software, pharmacy benefit management (PBM) systems, pharmacy systems, and patient portals.
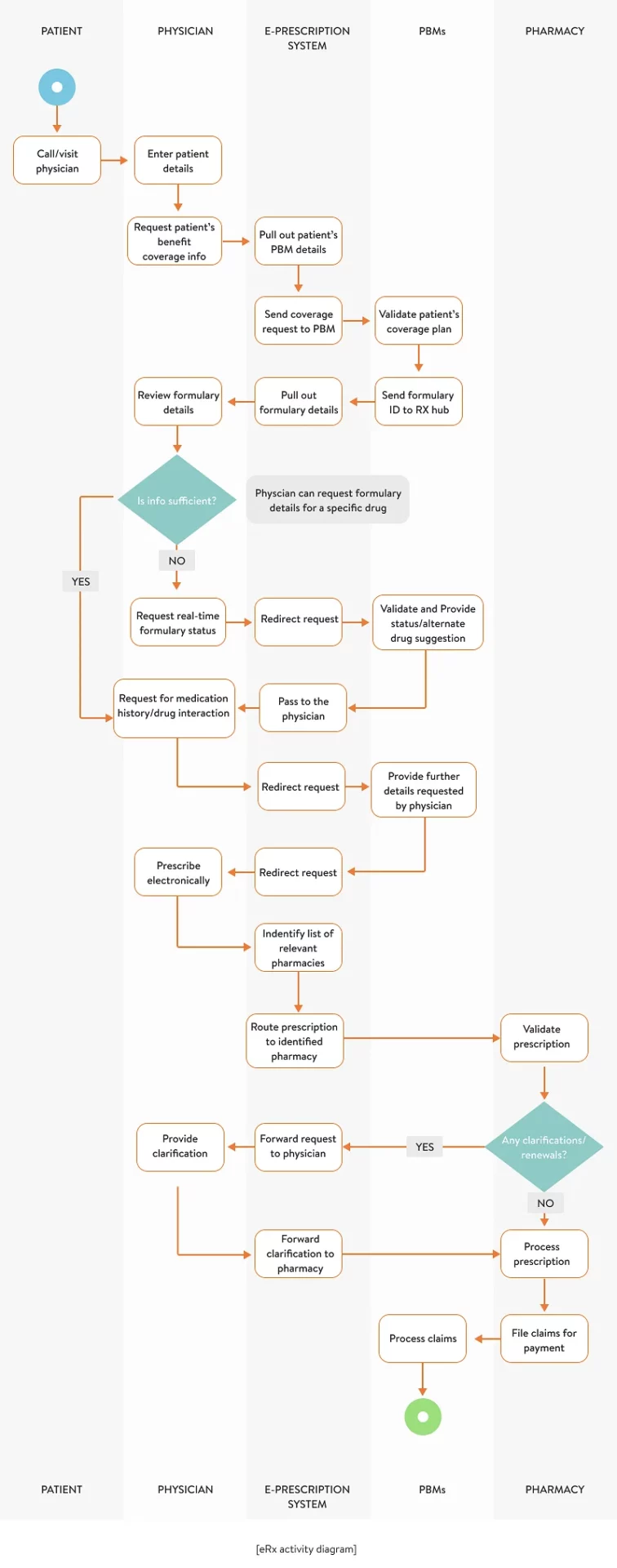
Based on the eRx activity diagram and illustrated information exchange, we’ve identified several indicators of whether your existing e-prescribing solution is effective:
#1 Basic security requirements
An eRx system works with sensitive health-related information. It retrieves, modifies, processes, and sometimes stores confidential user information such as patients’ treatment histories, private chats between doctors and pharmacists, and doctors’ geolocations. Therefore, an eRx system should comply with the Health Insurance Portability and Accountability Act (HIPAA).
These are some of the key technical safeguards that can’t be omitted while implementing an eRx system:
- Access control. According to the HIPAA Security Rule, access control is defined as “the means necessary to read, write, modify, and communicate data.” The Security Rule requires to enable different access levels with different access rights for each type of system so users can access the minimum necessary ePHI to successfully do their jobs. Even though the Security Rule does not state specific requirements for the type of access control method or technology to implement, we recommend setting up a unique user identification process while registering within the app — for example, by enabling a password or biometric login plus multi-factor authentication through custom-generated tokens sent via an SMS or app notification. An emergency access procedure is also a required technical safeguard to let users access ePHI in urgent situations or in the event of unexpected technical damage.
- Audit controls and activity logs in the case of an eRx system are required to define and register any activities associated with using ePHI. They also record any users’ operations with data after they access it.
- Addressable technical safeguards come with more flexibility than required safeguards but are still necessary to implement. They involve:
- a mechanism for authenticating ePHI to track any event associated with changing or destroying sensitive information in an unauthorized manner
- an advanced data encryption and decryption mechanism to decrypt all information that flows beyond the main application and its integrations, such as an EHR or pharmacy management software
- automatic logouts after a defined interval to increase security and avoid any unauthorized access to ePHI in case a device is left unattended, for example
How to use healthcare APIs to enhance your software security
Developers of healthcare software applications must pay close attention to ensuring security as these apps manage sensitive personal information. Its misuse can result in disaster, from stolen identities to a patient’s death. Developers have no option but to make sure their software complies with regulations, such as HIPAA (USA), PIPEDA (Canada), DPA (the UK and Spain), or GDPR (the EU).
API security must ensure multi-level data protection and provide effective threat prevention tools. Chino.io is one platform that promises the necessary level of security for healthcare enterprises and developers offering software for US and EU healthcare providers.
Chino.io complies with current EU regulations and the data protection laws of EU Member States. Chino.io provides proprietary technology and consulting services to ensure your apps are GDPR- and HIPAA-compliant. They also provide software quality certification according to security standards ISO 9001, ISO 27001, and ISO 13485, supporting the certification of medical-grade software and devices.
In general, healthcare solution development requires developers to take into account the following aspects of security:

Medical app development supported by additional healthcare APIs provides the following benefits:

#2 Local policies and authorized medications
Here’s how you can help your end users issue legal and authorized drug prescriptions:
Integration with the Drug Enforcement Administration security regulations:
An eRx system that lets providers prescribe controlled substances has to be certified as compliant with EPCS. Here’s a list of Drug Enforcement Administration (DEA) security requirements:
- Prescriber identity proofing. This security measure ensures that only DEA-certified practitioners can e-prescribe Schedule II–V drugs. There are two optional methods for identifying providers’ identities that are accepted by the DEA: institutional (the process of identity proofing must be conducted by DEA-registered institutional practitioners) and individual (practitioners must work with a digital credential service provider or an approved certification authority). ID.me and Imprivata are two of the most reliable identity proofing technology vendors on the US market that can be integrated with an eRx app, allowing EPCS-eligible providers to verify their identity through checking their legal identity information against NPI and DEA databases upon registering in the system.
- Two-factor authentication to e-sign digital prescriptions. The DEA has imposed several requirements for multi-factor authentication and digital signing for administrators of e-prescribing systems and prescribers. Multi-factor authentication provides an appropriate level of security when a prescriber signs a digital receipt in the e-prescription app, it confirms that the prescriber’s action is legitimate. Two of the following three authentication methods must be involved in your eRx system: a secure password/username, a hard token (must comply with FIPS 140 Security Level 1 for cryptographic devices or OTP devices), and biometric data. Your EPCS application must meet all the DEA requirements or else it won’t be certified by the DEA.
- Logical access control. You also need to set up a logical access control process within the system to grant EPCS permissions to authorized practitioners. There are essentially two individuals who must be involved in setting up logical access controls: the first individual must grant appropriate permissions in the EHR (for example, a system administrator) and the second must authenticate with the EMR to approve practitioners’ access level.
- Reporting functionality and an audit log provide clinicians and pharmacies with the ability to report directly to the DEA (in case of significant loss of a controlled substance, suspicious or illegal pharmacy or physician activity, etc.). Healthcare professionals can track all significant data related to the e-prescription process (who transmitted a certain prescription, when, and for what purpose). Thus, in case of any incidents or ADEs, it’s easy for providers to identify who’s responsible. It’s also possible to prove a patient’s eligibility for prescribed drugs and comply with the law.
In such a way, your eRx system can automatically keep up with DEA regulations so you don’t have to worry about it.
Integration with controlled substance databases
Prescription drug monitoring programs (PDMPs) have different rules and requirements in each state. Moreover, these rules and requirements are constantly being updated. That’s why there’s a strong need to simplify the process of tracking and giving prescriptions.
Integrating an eRx system with a PDMP provides rapid access to a state’s local X database and provides information from this database within a patient’s chart in the EHR system. By tracking a controlled substance database (CSD), physicians and pharmacists can:
- electronically prescribe controlled substances (Schedule II–V drugs) according to the requirements of each state
- review formulary details while prescribing controlled substances
- easily adapt to state-specific laws while administering, dispensing, or prescribing controlled substances
- manage a patient’s controlled substance use patterns per state
- regulate and identify patients under increased risk of becoming opioid-dependent
- coordinate patients to receive opioids from a verified provider in compliance with laws
Integration with a PDMP allows clinicians to:

Integration with the FDA database
The US Food and Drug Administration (FDA) is concerned with verifying medications. It evaluates risks related to medications, and ensures safety in compliance with applicable standards and labelling requirements. Thanks to automatic access to the FDA database, clinicians can:
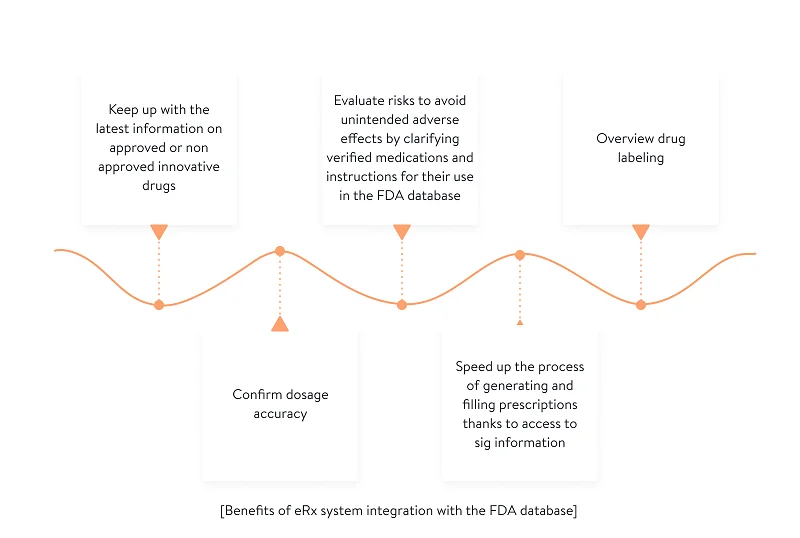
Thus, physicians can establish a safe and effective treatment plan before a prescription is transmitted to a pharmacy.
#3 Additional integrations
Below are some other valuable improvements that an eRx system needs to minimize medication errors:
Clinical decision support (AI and machine learning)
Through integrating medical prescription software with clinical decision support systems (CDSSs), you can increase patients’ safety and provide better treatment. Existing CDSSs analyze multiple pieces of health data to provide clinical advice. CDSSs combine health observations with doctors’ own knowledge and help doctors make informed decisions concerning patient treatment. There are two types of CDSSs: knowledge-based and non knowledge–based.
A knowledge-based CDSS usually consists of three ingredients:
- A knowledge base
- An inference engine
- A mechanism for communication
The knowledge base contains a set of rules and associations that work in accordance with the IF–THEN principle. For example, if your eRx system needs to check for a drug–drug interaction, the rule may be written as:

The inference engine then combines knowledge-based rules with a patient’s data to check for further tolerance beyond contraindications. The communication mechanism informs the prescriber of the results of analysis – for example, it can alert on a dangerous contraindication with a patient’s current treatment program or a potentially lethal drug dose. This technology is based on the GELLO or CQL (Clinical Quality Language) expression languages.
A non knowledge–based CDSS uses machine learning to analyze past experience in order to find common patterns in clinical data for better decision-making. However, these systems are often called black boxes since machine learning technologies can’t explain the reasons for their conclusions. That’s why non knowledge–based systems are used for post-diagnosis to check clinicians’ hypotheses.
With a knowledge-based CDSS, physicians are aware of drug interactions and allergies when writing electronic prescriptions. Clinicians can predict possible side effects thanks to a knowledge-based CDSS. Besides, an eRx system can send alerts to clinicians, pharmacists, and caregivers on contraindications, dangerous doses, potential adverse reactions, and duplicate therapies while providing clear instructions on how to ensure better treatment.
Integration with PBM and payer databases
Electronic pre-authorization to check a patient’s eligibility for certain drugs can help to avoid unpleasant surprises at the pharmacy (for example, when prescribed medications are not affordable for the patient). Having access to a patient’s insurance information allows physicians to see formulary lists and choose medications covered by a patient’s drug benefit policy. For example, a doctor can immediately see whether brand name drugs are available to a patient within their policy to offer a better quality of care.
Integration with an EHR system
Thanks to the integration between an eRx system and existing EHR software, clinicians can search for patients and view their medical data and treatment histories while giving prescriptions. Prescribing physicians can prevent the wrong or duplicate drug prescriptions by checking a patient’s age, weight, allergies, and diagnoses. Additionally, secure in-app chat between patients, pharmacists, and physicians can assist healthcare professionals by clarifying any details related to patients’ medical data and providing additional instructions about medications.
For instance, Allscripts is an EHR solution integrated with eRx software that allows clinicians to e-prescribe and refill medications, monitor patient adherence, and send messages via secure in-app chat.
Take into account that your EHR system, as well as your eRx system, should be implemented according to the requirements of the Office of the National Coordinator (ONC) for Health Information Technology. The ONC Health IT Certification Program requires healthcare software developers to engage their end users (medical staff) in thorough usability testing to ensure patient safety and improve the overall usability of products.
Yalantis has experience in achieving ONC Health IT Certification for Healthfully, an all-in-one enterprise healthcare solution, and integrating healthcare solutions with well-known EHR systems, such as Epic, Cerner, Athenahealth, and other systems.
Reasons for a lack of EHR interoperability and how APIs can address them
Despite developments in EHR technology and adoption, EHRs keep contributing to data silos that make interoperability a challenge. APIs are one of the most promising ways to address all the reasons behind the EHR interoperability mess.
Here are some of the main reasons for a lack of interoperability, data exchange, and data sharing across EHRs and other health information technology (HIT) systems:
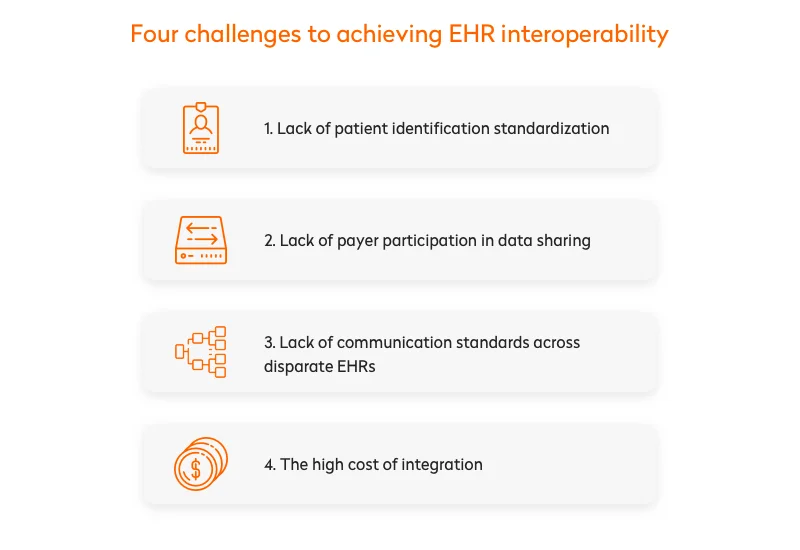
Lack of common patient identification standards. EHRs are the key repositories and ways to access patient information. But there’s still no national patient identifier helping us recognize a specific patient within an EHR system. Issues with identifying patients and matching their records are a huge problem for healthcare providers. The result is inflated healthcare expenses, poor quality of treatment, and safety issues.
Insufficient payer participation in data sharing. There’s a terrific amount of data in the hands of payers. Having access to this data would do healthcare providers a great service, facilitating health outcomes. But payers are protecting that data industriously, as it essentially contributes to their profits, and are shifting from public to private health information exchange. This makes it harder and more expensive for providers to ensure interoperability and integration.
Lack of communication standards across EHRs. Sharing clinical information between hospitals is gaining momentum. But multi-hospital systems and networks are increasingly sharing data between different EHR systems. EHR vendors often build proprietary communication and language protocols, which blocks communication with other EHRs. This requires healthcare providers to somehow integrate with multiple EHRs inside and outside their own facilities.
EHR integration is costly. Lots of medical institutions are using different medical technology systems to manage protected health information (PHI). This requires them to connect and integrate with disparate EHR and HIT systems. Ensuring such a level of connectivity is so costly that only large healthcare enterprises can afford it.
APIs have the potential to address all these problems by ensuring data and PHI sharing and communication between EHRs and HIT systems. Many of the big EHR vendors already offer open APIs to help third-party software developers build apps that access EHR data. But it’s not that simple! Due to technical, security, and regulatory barriers, integrating a third-party EHR is still a challenge.
Integration with pharmacy management systems
Providing eRx integration with pharmacy management systems helps to optimize doctors’ and pharmacists’ use of time, allows clinicians easy access to appropriate medications, and brings more data security. Physicians can clarify the availability of prescribed drugs in pharmacies, check their costs, track the order statuses of prescribed medications, and monitor medication adherence during all periods of treatment. Geo-awareness can also help doctors choose nearby pharmacies to send prescriptions to.
The best pharmacy management systems (such as Winpharm, Rx30 Pharmacy System, and PrimeRx) offer all of the abovementioned functionalities. For example, the Surescripts Network Alliance provides for the exchange of medical records, medical histories, and electronic prescriptions among clinicians, pharmacies, and pharmacy benefit managers.
Though e-Prescribing software development is mostly welcomed by physicians and clinical staff, there are still some challenges and a high rate of medication errors. That’s why clinicians and IT vendors might consider investing more resources into electronic prescription app development. Integrating an eRx with other systems can be the best choice to increase the value of your e-prescribing software.
If you want to build an efficient eRx system that delivers mature, safe, and high-quality care, Yalantis is here to answer all of your questions.
Rate this article
5/5.0
based on 1,177 reviews